Abortion
Table of Contents:
- Spontaneous Abortion vs. Intrauterine Fetal Demise
- Abortion
- Recurrent Pregnancy Loss
- Anti-D Immune Globulin
- Threatened Abortion
- Inevitable Abortion
- Incomplete Abortion
- Complete Abortion
- Missed Abortion
- Septic Abortion
- Boggy Uterus
- Overall Approach to Abortion
There are several key subtypes of spontaneous abortion that we need to be aware of for examinations.
These include all the types pictured below as well as the septic abortion, all of which we will cover in detail.

However, before we discuss each type of spontaneous abortion individually, we will first need to discuss some key principles which pertain to abortion in general.
Spontaneous Abortion vs. Intrauterine Fetal Demise
One important thing to establish before we begin our discussion of spontaneous abortion is to be able to distinguish between spontaneous abortions and intrauterine fetal demise.
 ©2019 BoardsMD
©2019 BoardsMD
An intrauterine fetal demise is a fetal death which occurs at 20 weeks or more of gestation.
It is important that we use this landmark of 20 weeks. As fetal deaths, which occur at 20 weeks or more of gestation will be intrauterine fetal demise, abbreviated here as IUFD.
Those that occur at less than 20 weeks will be spontaneous abortions, which is the focus of the remainder of this module.
Abortion
The definition of an abortion is a termination of pregnancy at less than 20 weeks gestation or at a weight that is less than 500 grams.
Pathophysiology
It is important to recognize that the most common cause of abortion is chromosomal abnormalities, especially during the first trimester.
Additional causes of abortion include antiphospholipid antibodies as we see in lupus infections as well as anatomic anomalies especially those that involve the uterus or the fallopian tubes.
Diagnosis
In actual clinical practice, the diagnosis of abortion relies on several modalities, including the physical exam, ultrasound, and the use of B-hCG measurements.
However, often in patient vignettes, you will need to rely on three key components in order to clinch the diagnosis of abortion for the purposes of examinations.
These components include whether the following are present:
- vaginal bleeding
- cervical dilation
- products of conception present in the vaginal canal.
As we move through the various subtypes of abortion, you will be able to recognize these three key components with ease and use them to distinguish between the various types of spontaneous abortions.
Managing Spontaneous Abortions
As we move through each individual type of abortion, we will discuss the various principles of management for the specific subtypes in detail.
However, I would like to make it clear here that there are really three key management pathways when it comes to managing spontaneous abortion.
These include:
- Expectant management in which we monitor the patient with regular follow-up, but give no pharmacologic or surgical interventions.
- Medical management in which we can use a combination of Mifepristone, and Misoprostol. This is the most common regimen for spontaneous abortion in the United States or in some cases we can use Methotrexate.
- Surgical management including the use of the dilation and curettage (D&C). In recent years, it has become increasingly common to use a dilation and evacuation (D&E) also known as a “Suction and Curettage”
Below we have an example of a dilation and curettage.

©2019 BoardsMD
As you can see in the image, we have a weighted speculum, which opens up the vaginal canal in a downward direction.
This allows us to use a curette in order to essentially scoop out the contents of the dead fetus from the uterus.
This is what a dilation and curettage looks like.
Alternatively, in a dilation and evacuation or suction curettage, rather than using this curette you will instead see the use of a vacuum or suction instrument.
This is a procedure that you will often see in questions, but also commonly under OBGYN rotations.
Recurrent Pregnancy Loss
Another important principle to be aware of in the context of spontaneous abortions is recurrent pregnancy loss.
By definition, recurrent pregnancy loss is when a female patient has at least three consecutive spontaneous abortions.
Pathophysiology
As we discussed previously, the most common pathophysiology of spontaneous abortion is chromosomal abnormalities.
Therefore, as part of our workup, we will need to get a karyotype in order to have an analysis of both the products of conception, as well as the parents' DNA.
This will ultimately be done in order to look for chromosomal anomalies.
Additionally, these patients will undergo a hysterosalpingogram (HSG) in order to look at the anatomy of the uterus, as well as the fallopian tubes.
We have an example of a hysterosalpingogram below where you can see that this dye has been injected in order to demonstrate that indeed, these fallopian tubes are Peyton.

If they were scarred over, for example in a patient with a history of pelvic inflammatory disease, then we wouldn't be able to see this contrast material flowing freely through these fallopian tubes.
In patients with recurrent pregnancy loss, it is also standard to get lupus anticoagulant studies in order to look for the presence of antiphospholipid antibodies as seen in the antiphospholipid antibody syndrome common in patients with lupus.
Anti-D Immune Globulin
It is important to recognize the indications for the use of Anti-D Immune Globulin.
The indications for Anti-D Immune Globulin include:
- Routine prenatal care at 28 to 32 weeks.
- Delivery of an RH-(+) baby
- Ectopic pregnancy
- Abdominal/Pelvic trauma in a pregnant woman
- Second and third trimester bleeding
- Invasive screening methods including amniocentesis and chorionic villus sampling
- External Cephalic Version
- Abortion
It is important to recognize that abortion is an indication for the use of Anti-D Immune Globulin in those patients who are at risk for ISO immunization.
Threatened Abortion
This will occur in a pregnant woman who has less than 20 weeks gestation as that is our cutoff for spontaneous abortion, as opposed to intrauterine fetal demise.
These patients in board vignettes will present with vaginal bleeding, a closed cervix, as well as no products of conception present in the vaginal canal.
We have a schematic of this below, where you can clearly see that there is the presence of vaginal bleeding, the cervix is closed, and there are clearly no products of conception in the vaginal canal.

It is almost as if the fetus, which is still present within the uterus is threatening to abort, hence the name threatened abortion.
However, with the cervix closed and no products of conception present in the vaginal canal, we cannot say that this is an inevitable abortion or that this is an incomplete abortion.
We still have the products of conception present within the uterus and therefore this is only a threatened abortion.
Diagnosis
When we perform our speculum examination, there will be bleeding present in the vaginal canal.
However, there will be no products of conception in the vaginal canal.
Classically on ultrasound in these patients, we will be able to see a viable fetus with a fetal heartbeat. This is consistent with a threatened abortion, which will not necessarily result in an actual, full-blown abortion.
Management
In these patients, the next step in management is going to be expectant management, as well as Pelvic Rest so that we do not disturb this viable fetus that is still present within the uterus and still has a chance of survival.
In addition, we will need to get serial Beta-hCG measurements in these patients in order to monitor these threatened abortions for possible progression to the next type of spontaneous abortion.
Inevitable Abortion
Consistent with the definition of a spontaneous abortion, this will occur in a pregnant woman who has less than 20 weeks gestation.
The patient will present with bleeding and cramping, a dilated cervix, and no products of conception in the vaginal canal.
As we take a look at the schematic below, we can see that there is indeed bleeding into the vaginal canal.
Additionally, there are no products of conception in the vaginal canal.

However, we need to note here that the cervix is indeed open.
Therefore, one could argue that if there is vaginal bleeding, as well as an open cervix, that is essentially inevitable that abortion is going to occur. Hence the name inevitable abortion.
Diagnosis
When we perform a speculum exam in these patients, we are going to see blood, but no products of conception present in the vaginal canal.
On ultrasound in these patients, we will see a gestational sac that is present in the lower uterus.
This should really make sense to us in the context of an inevitable abortion because one can imagine that the products of conception of the fetus are present in the lower uterus and essentially pushing up and opening the cervix. From here, it is inevitable that an abortion will occur at some point in time.
Management
In these patients, if fetal heart tones are still present, then there is still a chance of this fetus surviving and therefore we proceed with expectant management.
However, if fetal heart tones are absent, we can proceed with medical management using Misoprostol in combination with Mifepristone.
If the patient is unstable and is hypotensive and tachycardic, then we can give these patients IV Fluids and proceed with a Suction Curettage procedure in order to remove the fetal contents and prevent our patients from progressing to more serious complications, such as a septic abortion.
Incomplete Abortion
Our patient is going to be a pregnant woman who has less than 20 weeks gestation.
She will present with vaginal bleeding and cramping as well as a dilated cervix.
So far, this is similar to inevitable abortion. However, in the case of an incomplete abortion, there will be products of conception present in the vaginal or endocervical canal on physical exam.

Therefore, we can now state with certainty that this is not simply an abortion that is inevitable, but rather it is an incomplete abortion, where some products of conception are still remaining within the endometrial cavity. Whereas other products of conception have already made their way into the endocervical and vaginal canal.
This is the hallmark of incomplete abortion.
Diagnosis
On speculum exam, these patients will have products of conception in the vaginal canal.
Additionally, on ultrasound, because there may still be some remaining products of conception within the endometrial cavity, these patients may or may not have products of conception on ultrasound still present in the uterus.
Management
As is typical for our management of spontaneous abortion in general, if a patient with an incomplete abortion is stable, then we can proceed with medical therapy, including Misoprostol and Mifepristone.
However, if the patient is unstable, then we can give IV Fluid Resuscitation and proceed with a Suction Curettage in order to remove the remaining fetal contents and prevent potential progression to septic abortion and other complications.
Complete Abortion
This will be a woman who is less than 20 weeks gestation.
The patient may or may not recall having a history of vaginal bleeding,
The patient will have a closed cervix.
Because this is a complete abortion, the products of conception will be completely expelled. Therefore, there may even be a visible mass protruding into the vagina.
This is consistent with the schematic below where we can clearly see that there are no remaining products of conception in the endometrial cavity. Rather there are products of conception which are now present in the vaginal canal.

This is what distinguishes an incomplete abortion where we may still have some products of conception in the endometrial cavity, from a complete abortion in which these products of conception have been entirely expelled.
Diagnosis
In addition to a visible protruding mass in the vaginal canal, on speculum exam, we may also sometimes see blood present in the vaginal canal.
If we were to perform an ultrasound, we would see that the endometrial cavity is empty, consistent with the fact that this is a complete abortion and the products of conception have been completely expelled.
Management
To our knowledge, in these patients the products of conception have been completely expelled and therefore we can proceed with expectant management and monitoring of serial Beta-hCG. The idea here being that there are no remaining products of conception and therefore we do not need to worry about remaining products proceeding to septic abortion or other complications.
However, if we feel that there are indeed remaining products of conception that may be present in the endometrial cavity, then we can proceed with a suction curettage.
Missed Abortion
This will be a pregnant woman who is less than 20 weeks gestation and it will present with a loss of early pregnancy symptoms.
In normal pregnancy, women have several physiologic changes. One of the most common is nausea.
One of the presentations of a missed abortion is for a patient to initially have nausea or other symptoms of early pregnancy and to lose these symptoms, raising our suspicion that we may have missed an abortion in this patient.
For the purposes of examinations these patients will typically present with;
- no vaginal bleeding
- a closed cervix
- no products of conception in the vaginal canal
This is consistent with our image below where we have a dead fetus still present inside the endometrial cavity.

Cervical dilation and vaginal bleeding will be absent in patients with a missed abortion.
Diagnosis
When we perform a speculum exam in patients with a missed abortion, we will see no blood and no products of conception present in the vaginal canal.
Instead, if we were to perform an ultrasound in these patients, we would see that there are still products of conception present in the uterine cavity, not the vaginal canal.
We would also see that these patients have an absence of fetal cardiac activity indicating that the fetus remaining in the uterus is no longer viable and that we have indeed missed the abortion.
Management
These patients have multiple options in terms of their management.
We can proceed with expectant management, with serial Beta-hCG monitoring, and wait for the patient to dispel this dead fetus
However, if the patient and physician decide together that they want to remove this dead fetus then we can proceed with a suction curettage.
Septic Abortion
Our patient would be a pregnant woman.
She will present with fever and abdominal pain.
In addition, these patients will have a recent history of an elective abortion or a history of a missed/incomplete abortion.
This is consistent with the underlying pathophysiology of septic abortion.
Pathophysiology
Septic abortion is most commonly a non-sterile elective abortion.
In this case, there are going to be retained products of conception, which ultimately become infected leading to the development of a septic abortion, which is very much a feared complication of spontaneous abortions and is considered to be a medical emergency
On physical exam, patients with a septic abortion will classically have a dilated cervix.
When we perform our speculum exam, they will have a purulent, bloody, and malodorous discharge.
Additionally, because the pathophysiology of a septic abortion is retained products of conception, we will be able to see these retained products of conception on ultrasound.
This may also be described on ultrasound as having a thickened endometrial Stripe.
Management
If we suspect endometritis in a patient with a septic abortion, then we should ultimately obtain blood and endometrial
After attaining these cultures, we can treat these patients first with broad spectrum antibiotics and after we begin antibiotic therapy we can proceed with a suction curettage in order to remove any remaining products of conception that may be infected and leading to this septic abortion.
Boggy Uterus
Boggy Uterus is a term that is commonly used in OB/GYN question stems.
When we say boggy, we are referring to something that is soft and flaccid.
There are three scenarios where we see this in question stems when it comes to obstetrics and gynecology.
The first classic scenario, which we see in the setting of postpartum hemorrhage is Uterine Atony, which we discuss in detail in our postpartum hemorrhage section.
We can also classically see a boggy uterus in our patients with Adenomyosis
You can also see this soft flaccid boggy uterus in question stems in the context of patients with septic abortion.
Overall Approach to Abortion
In this series, we have covered several high yield subtypes of spontaneous abortion including those which are pictured below, as well as the septic abortion.
Included here are some of the high yield take-home points for each type of spontaneous abortion in order to help you distinguish between our different subtypes:
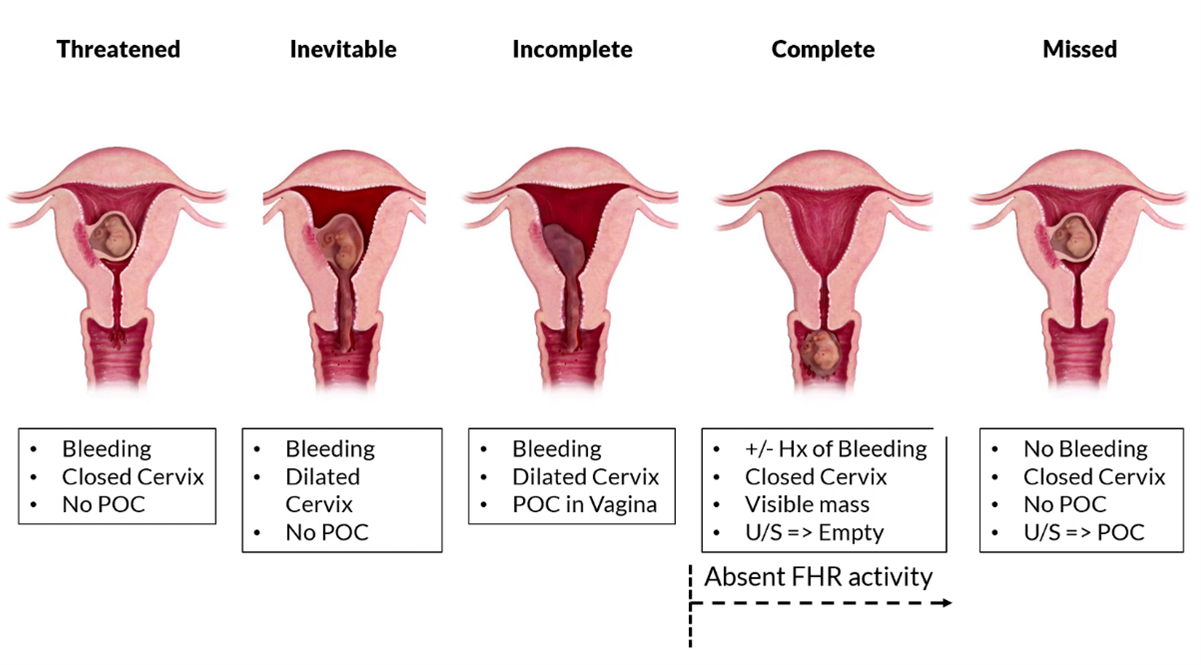
In a threatened abortion, we will see vaginal bleeding. However, the cervix is closed and there are no products of conception in the vaginal canal.
In inevitable abortion, the abortion is inevitable and therefore we will see vaginal bleeding, a dilated cervix. However, there are no products of conception in the vaginal canal.
In an incomplete abortion, we will see vaginal bleeding, a dilated cervix and because this is an incomplete abortion, some products of conception will be in the vaginal canal and some products of conception will still be remaining in the endometrial cavity.
In a complete abortion, the products of conception are no longer present in the endometrial cavity. And now these products of conception are in the vaginal canal, classically as a visible mass.
In a missed abortion the patients have a dead fetus that is still present within the endometrial cavity. This is something that we will be able to see as a finding on ultrasound as either retained products of conception or a thickened endometrial stripe.
It is also important to keep in mind that once we reach the point of a complete or a missed abortion that there will be an absence of fetal heart rate activity.
As at that point, we have reached the point of no return where there's really no chance of survival of the fetus.
If you simply keep in mind the three key features of vaginal bleeding, cervical dilation, and products of conception in the vaginal canal, then you will be well on your way to diagnosing and differentiating the various subtypes of spontaneous abortion.
Stay connected with news and updates!
Join our mailing list to receive the latest news and updates from our team.
Don't worry, your information will not be shared.

