Contraception
Table of Contents:
- Choosing the Correct Form of Contraception for Your Patient
- Barrier Contraception
- Hormonal Contraception
- Oral Contraceptive Pills
- Injections
- Implants
- IUDs
- Sterilization
- Approach to Contraception
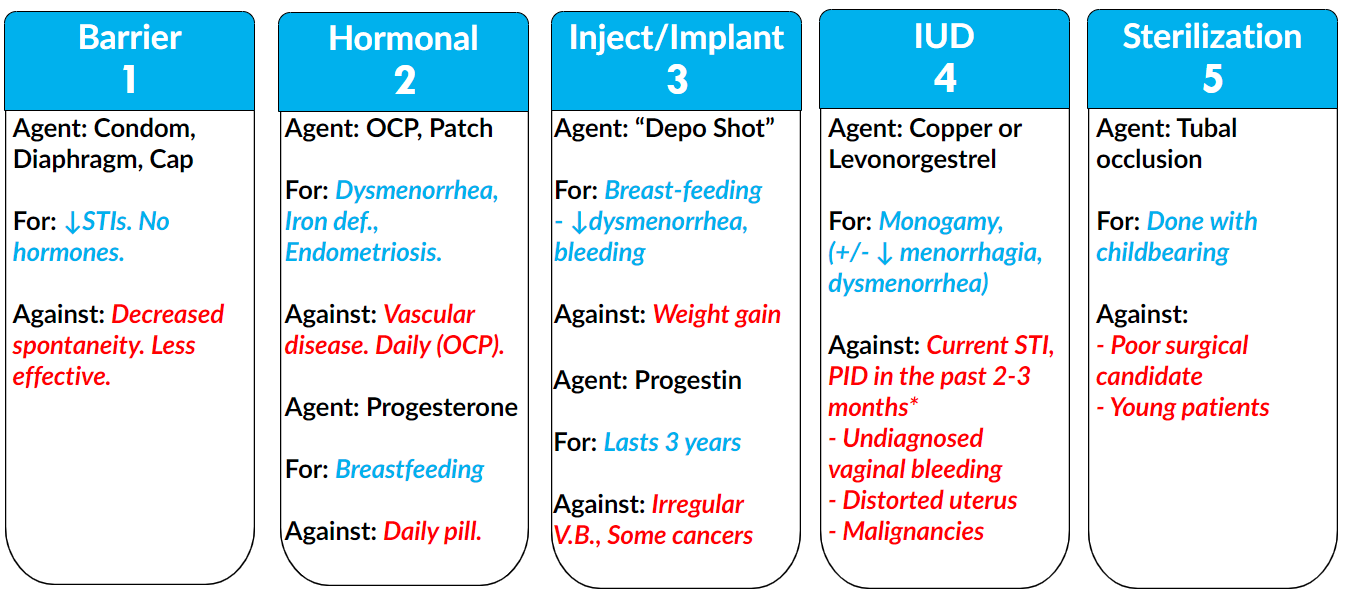
There are several high yield types of contraception that we need to cover.
Before we discuss each method of contraception individually, let's first start by forming a framework for how to approach contraception and how to select the correct method in our given patient.
Choosing the Correct Form of Contraception for Your Patient
For the purposes of examinations if we simply know the answers to 4 key questions, then we can easily select the correct answer choice and determine the correct type of contraception for our particular patient.
These four questions are:
- Does the patient desire STI protection?
- Does the patient have any contraindications to hormonal therapy including estrogen and progesterone?
- Does the patient have an active STI or a recent episode of pelvic inflammatory disease?
- Does the patient desire future children? This is very important for OBGYN, especially on examinations.
If you simply keep these four key questions in mind, as you approach various exam questions, then you will have no trouble at all In selecting the correct answer.
Barrier Contraception
This includes the male and female condom as well as the cervical diaphragm and cervical cap.
For the purposes of examinations, the male condom is far more likely to be the correct answer.
As we have hinted at already, the mechanism of barrier contraception as evident in the name barrier is that these methods will form a physical obstruction.
Advantages
There are some key advantages to utilizing barrier contraception.
This method decreases transmission of STIs. Very high yield to keep in mind is that a decrease in transmission of STIs is unique to the barrier contraceptives in comparison to other contraceptive agents.
They do not utilize hormones in order to work. As we will see moving forward in these lessons, there are some patients who have contradictions to hormonal therapy and therefore this aspect of having no hormones is extremely important to keep in mind.
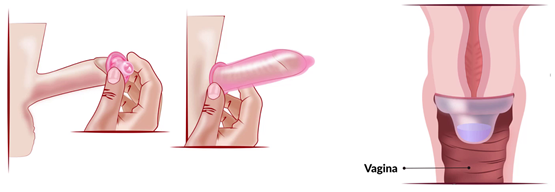
Below, you can see that we have a male patient putting on a male condom. If this patient were to ejaculate, the semen would be confined within this condom and would not be able to escape and ultimately go into the female patient.
©2019 BoardsMD
There's a similar concept with the cervical diaphragm and cervical cap in that these act as a physical barrier against the passage of semen preventing the semen from reaching the uterine cavity and thus preventing possible pregnancy from occurring.
Disadvantages
There are still some important cons of the use of barrier contraception.
Some patients may form allergic reactions or may have irritative contact dermatitis in response to barrier contraceptives.
The fact that the patient has to stop and put on a condom or stop and put in a diaphragm or a cervical cap results in decreased spontaneity or decreased pleasure on the part of the patient and in some cases, this can lead to non-compliance.
For those patients who desire the utmost in terms of contraceptive benefit and the lowest possible chance of having a pregnancy, barrier contraceptives are actually less effective in comparison to IUDs which have the highest rate in terms of preventing unwanted pregnancy.
Another potential side effect although rare is that if the cervical diaphragm is left in for too long it can result in toxic shock syndrome. Toxic shock syndrome is most frequently tested in the context of nasal packing as well as leaving in tampons. However, the syndrome has also been reported in patients who have left in a cervical diaphragm for too many hours.
Hormonal Contraception
These hormonal methods of contraception include those which utilize estrogen and progesterone together, as well as those which utilize only progesterone. We will begin first with combined hormonal contraceptives.
Combined E + P
When it comes to contraceptives, which combine both estrogen and progesterone together, we have several agents that we can utilize the most common of, which is combined oral contraceptives.
Estrogen and progesterone can also be given in the form of the patch as well as a vaginal ring.
The major mechanisms of these agents are to thicken cervical mucus, which prevents sperm from passing through into the uterine cavity, as well as thinning the endometrial lining.
In the case of both of these mechanisms, these are both primarily mediated by the progesterone within these agents.
There are several benefits to the use of combined estrogen and progesterone hormonal agents, which helps to explain why combined oral contraceptives are so commonly used.
Advantages
Benefits for many patients include that these agents can help to decrease dysmenorrhea or pain with periods
decrease bleeding during periods therefore decrease anemia.
In some patients who are struggling with hirsutism, combined oral contraceptives can also be quite helpful. We classically see this used in our patients with PCOS.
It has also been demonstrated that combined hormonal contraceptives help to decrease the risk for the development of ovarian and endometrial cancer.
These agents also decrease the risk of developing pelvic inflammatory disease, fibrocystic change of the breast as well as osteoporosis.
Disadvantages
These benefits of combined hormonal agents are not without their drawbacks.
One of the major issues with the use of these agents is the necessity of compliance as these agents must be taken every single day.
If the patient does not take these agents within the same three-hour window each and every day, then they lose their efficacy and the patient can inadvertently become pregnant.
These agents should also be avoided in any patient with a history of a thromboembolic event, coronary artery disease, cerebrovascular accident, uncontrolled hypertension, retinopathy, or nephropathy. This is because these hormonal agents have been demonstrated to increase the risk of thromboembolic events, coronary artery disease, and even stroke.
This is also why these agents are contraindicated in smokers who are over the age of 35, as well as patients who have a history of migraine with aura.
Patients with normal migraines are able to take these agents.
Those who have migraine with aura have been demonstrated to have an increased risk for the development of thromboembolic events. These contraindications are something that frequently shows up on examinations.
These agents should also be avoided in patients who have undiagnosed vaginal bleeding.
©2019 BoardsMD
They should also be used in caution with patients who are using P450 inducers as OCPs, can have decreased efficacy when used in conjunction with these agents.
The combined hormonal patch has been shown to have decreased efficacy in patients who weigh more than 200 pounds and therefore this method should be used with caution in these particular patients.
Oral Contraceptive Pills
Above we have a schematic of how oral contraceptive pills are normally packaged. As you can see the way that these pills are laid out, we have seven in each row in order to help the patient to be compliant and to take these each and every day at the same time.
This is because failure to do so can ultimately render these agents ineffective and the patient can inadvertently become pregnant.
Progesterone
In addition to combined hormonal contraceptives, we also have progesterone only agents including the most common of which is the progesterone only “mini pill”.
The progesterone only mini pill works via progesterone mediated mechanism by thickening cervical mucus, and by thinning the endometrial lining.
Advantages
One major advantage of these progesterone only mini pills is that they can be used safely in patients who are breastfeeding. This is in contrast to agents which contain estrogen, which is believed to alter the contents of breast milk.
Therefore, for patients who are breastfeeding, we should favor progesterone only agents rather than combined oral contraceptives.
Progesterone, only agents are also helpful in that unlike their combined counterparts, which contain estrogen, they lack the estrogen component, which increases the risk of thromboembolic events.
Therefore, the restrictions in smokers over the age of 35, as well as patients with a history of thrombotic events, don't apply for the case of progesterone only agents.
Disadvantages
Much like their combined estrogen and progesterone counterparts, patients are required to take these progesterone only agents at the same time every day. Otherwise these agents will be rendered ineffective.
Injections
One injection you'll see on examinations but which is also very common clinically is Depot Medroxyprogesterone Acetate injection (Depo Shot).
Because this injection contains medroxyprogesterone it is going to work via progesterone mediated mechanism. The Depo shot will inhibit ovulation, thicken cervical mucus and thin the endometrial lining.
Therefore, the Depo shot is extremely similar to our progesterone only mini pill and has many of the same advantages.
Advantages
The Depo shot could be used safely in patients who are breastfeeding as it does not contain any estrogen, which is believed to compromise the breast milk.
It should be noted however, that unlike the progesterone mini pill, which must be taken every day, the Depo shock can be given once every three months.
Therefore for many patients, they prefer this from a compliance perspective and that they can simply go in for their shot every three months, and then not have to worry about taking a pill every single day.
Other benefits of the progesterone within these injections include that these Depo shots can;
- decrease dysmenorrhea
- decreased vaginal bleeding during periods
- decrease anemia
- decrease sickle cell pain
- decrease the risk of seizures.
Disadvantages
It can cause weight gain which is very undesirable for a lot of patients.
The Depo shot has also been shown to increase the risk of depression in select patients and increase the risk for osteoporosis.
Implants
When it comes to examinations, the one implant that you need to be aware of is the Progestin implant which secretes Etonorgestrel.
This implant is going to work via progesterone mediated mechanism by inhibiting ovulation, thickening cervical mucus, and thinning the endometrial lining.
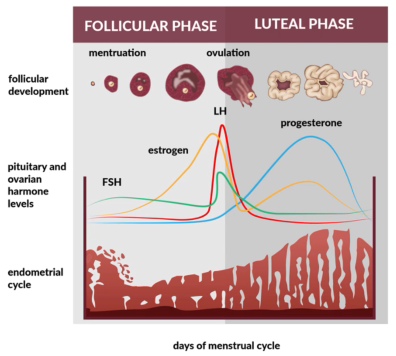
And if we look back to our basic sciences in terms of the menstrual cycle, this should make sense. As far as progesterone's effects on the uterus, go during the luteal phase of the menstrual cycle, progesterone levels reach their peak as demonstrated below by this blue line.
©2019 BoardsMD
The downstream effect of this rise in progesterone is ultimately going to be shedding of the endometrial lining as shown above during the menstrual period. This thinning of the endometrial lining, as well as thickening of cervical mucus and inhibition of ovulation, is what allows these progestin-based implants, as well as our progesterone-only pill and other progesterone mediated forms of contraception to take effect.
Advantages
This is excellent for mothers who are breastfeeding as they do not contain estrogen which can ultimately alter the contents of the breast milk.
These implants have an added benefit and that they actually last for three years, which is an advantage over the Depo shot which must be given every three months.
These progestin implants can further benefit patients by decreasing dysmenorrhea, bleeding, and anemia.
Disadvantages
They can increase irregular vaginal bleeding, therefore these agents are relatively contraindicated in patients who have undiagnosed vaginal bleeding.
These agents are relatively contraindicated in patients who have a history of thromboembolic disease, liver disease, or breast cancer.
IUDs
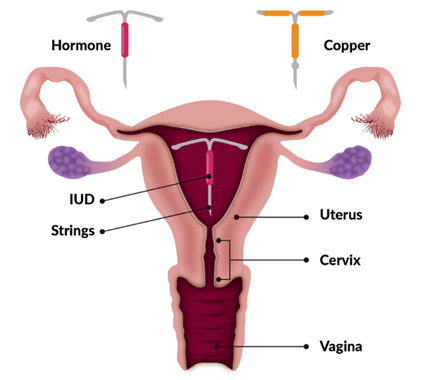
There are two types of IUDs that we can ultimately use in a given patient.
These include the Copper IUD, as well as the Hormone Secreting IUD as shown below.
This hormone secreting, IUD secretes progesterone and therefore it will have many of the same advantages and disadvantages as other progesterone based contraceptive forums.
©2019 BoardsMD
They can then remain in the endometrial cavity for five to 10 years, depending on the type of IUD. One of the key advantages of both of these types of IUDs is that they can be placed in the endometrial cavity.
This is extremely convenient for patients because in comparison to for example, oral contraceptives which must be taken every day, Depo shots which must be administered every three months or barrier contraceptives that must be used each and every time that the patient has intercourse, these IUDs are far more convenient.
Copper IUD
This instrument works by inhibiting sperm migration.
It achieves this by causing local inflammation.
Advantages
Fortunately, this agent does not utilize any hormones and therefore for patients who have contraindications to hormonal therapy, the copper IUD can be extremely ideal.
Other advantages of the copper IUD include that this agent can last for five years. This is extremely convenient in comparison to some of the other contraceptive options.
The copper IUDs is ideal for patients who are in long-term monogamous relationships. This is particularly true because the copper IUD as with the progesterone IUD does not provide any sort of barrier against STIs.
Therefore, in an ideal scenario, patient should be in a relationship with a partner who they can trust, if they're going to use an IUD and to go through everything that comes with having this implanted in their uterus.
The copper IUD is also excellent in terms of emergency contraception, as it begins working immediately.
Disadvantages
The copper IUD is ideal for patients who are in long-term monogamous relationships. Part of the reason for this is that one of the contraindications for using a copper IUD is having a current STI or an episode of pelvic inflammatory disease in the past two to three months.
This is because the IUD can ultimately act as a nidus for the infection and can prevent the patient from improving with antibiotic therapy.
Other relative contraindications for the use of the copper IUD include:
- Undiagnosed vaginal bleeding
- Malignant gestational trophoblastic disease
- Cervical endometrial or breast cancer
- Distortion of the uterine cavity for e.g. fibroids
As we could imagine if you were to have a submucosal or pedunculated fibroid that was poking into the endometrial cavity, it could be more difficult to place the IUD properly.
Wilson's disease is a contraindication for the placement of copper IUDs as these patients are already overloaded with copper in their bloodstream.
Levonorgestrel IUD
This is going to work via a progesterone-mediated mechanism by thickening cervical mucus and thinning the endometrial lining.
Advantages
Benefits of the Levonorgestrel IUD is the fact that it is long lasting, lasting for five years.
The Levonorgestrel IUD is best reserved for patients in long-term monogamous relationships with a partner that they can trust.
Additional benefits with the Levonorgestrel IUD include decrease in menorrhagia as well as a decrease in dysmenorrhea via progesterone mediated mechanism.
Disadvantages
The contraindications to Levonorgestrel IUD are similar to the copper IUD in that this agent should not be used if the patient has a current STI or has had an episode of pelvic inflammatory disease in the past two to three months.
This highlights the need for patients who have one of these IUDs placed to be in a stable long-term monogamous relationship with a partner that they can trust.
Other relative contraindications include;
- Undiagnosed vaginal bleeding
- Malignant gestational trophoblastic disease
- Cervical, endometrial, or breast cancer
- Distortion of the uterine cavity
Sterilization
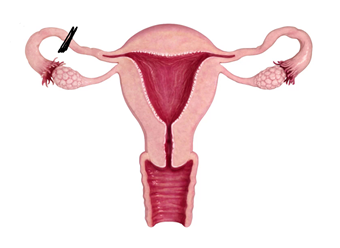
Sterilization is achieved via bilateral tubal occlusion.
The idea here, being that if we simply cut off the fallopian tube via ligation, then it will prevent a fertilized zygote from being able to pass in order to implant in the uterus in the endometrial cavity.
©2019 BoardsMD
The mechanism, therefore, is obstruction of the fallopian tubes.
This is going to be most ideal for patients who do not desire future children.
Disadvantages
Sterilization, however, with this bilateral tubal ligation is not going to be ideal for poor surgical candidates e.g., patients with severe coronary artery disease or morbid obesity.
Another alternative is hysteroscopic occlusion. This method of sterilization is supposed to come off of the market within the next year, so it is unclear whether this will be fair game in terms of examinations.
One other alternative is male sterilization. For patients who are poor surgical candidates but who have a male partner who is amenable to having himself sterilized, this can be a highly effective option.
Another major issue with sterilization is that some patients who may want to have sterilization performed at one point may later decide that they want future children. Therefore, with this elective procedure it is very possible that patients can feel an intense sense of regret if they ultimately go through with this.
This risk of having this regret is ultimately highest in the younger patients E.g. female patients who are in their teens or twenties.
Therefore, the pros and cons of the procedure, as well as the difficulty in trying to reverse sterilization procedures must be discussed with all patients, especially those who fall into this younger demographic. This is a topic that is frequently tested on examinations.
Approach to Contraception
©2019 BoardsMD
We have covered a significant amount of ground in these modules in terms of better understanding the pros, the cons, the mechanisms, as well as the agents of the various types of contraceptives
However, I do want to hammer home one point which is, that if we simply ask four key questions in terms of the patient's characteristics when choosing a contraceptive, we will ultimately be able to arrive at the correct answer choice on examinations.
- If the patient desires STI protection, then the contraceptive of choice is barrier contraception. The most likely choice on an examination is going to be the condom, specifically, the male condom.
- Does the patient have any contraindications to hormonal therapy? This includes being a smoker over the age of 35 or having a history of thromboembolic disease. These patients should ultimately get non-hormonal contraceptives. Options include barrier contraceptives as well as the IUD, especially the copper IUD.
- Does the patient have an active STI or a recent episode of PID for these patients? We need to avoid the use of IUDs therefore reasonable choices for contraceptives include barrier contraceptives, hormonal contraceptives, injections, or implants.
- Does the patient desire any children in the future? For these patients, if they are 100% certain that they do not want future children and particularly if they are not in their teens or twenties and likely to regret their decision of sterilization, then we can ultimately offer these patients a tubal occlusion.
Stay connected with news and updates!
Join our mailing list to receive the latest news and updates from our team.
Don't worry, your information will not be shared.

