Genetic Screening Methods
Table of Contents:
- Genetic Disease Screening
- Maternal Serum Screen
- Quad Screen Interpretation
- AFP
- Screening for Aneuploidy
- Cell-Free Fetal DNA
- Drawbacks
- Ultrasound
- Biophysical (BPP)
- Chorionic Villus Sampling (CVS)
- Amniocentesis
- Anti-D Immunoglobulin
- Summary
In this article we will discuss Genetic Screening methods that we use throughout pregnancy.
I love how high yield this article is, in that we really dive into a lot of key modalities that you see casually mentioned in question stems that are often not really clarified or well explained at the medical student level.
These include:
- Genetic Disease Screening, which for examination purposes, we will most commonly see in the context of cystic fibrosis, as well as sickle cell disease.
- Maternal Serum Screen which as we will see is performed in all patients, looking for AFP, B-hCG, Estriol and Inhibin, in order to identify aneuploidy, as well as ventral wall defects and other disorders, which we will cover here in detail.
- Cell-free Fetal DNA Testing, which is a noninvasive test that has become increasingly popular.
- Ultrasound
- Chorionic Villus Sampling - invasive testing procedure
- Amniocentesis - invasive testing procedure
Genetic Disease Screening
As genetic testing becomes increasingly accessible and popular in the modern age, we will likely see more and more diseases which are screened for in the coming decades.
However, at this point, for examination purposes, there are really just two key disorders which we need to be concerned with:
- Cystic Fibrosis
- Sickle Cell Disease.
When it comes to cystic fibrosis screening, this is essentially done universally in all Caucasian patients as we look for the ΔF508 mutation.
The way this usually works in practice is that the mother will be screened for this mutation. If the mother is positive, then we will do additional screening for her partner. If both parents are positive, then we can offer additional confirmatory diagnostic testing.
Unlike in cystic fibrosis, in which we are looking for a point mutation. For sickle cell disease screening, we perform Hgb electrophoresis in our African American patients.
This follows a similar algorithm to our cystic fibrosis screening as we first screened the mother. If the mother is positive, we then screen the partner.
If both parents are positive, then we can offer additional confirmatory diagnostic testing.
Maternal Serum Screen
The maternal serum screen is something that is offered to all Pregnant Patients.
This is offered to all patients as a screening system for aneuploidy and is especially important in our patients who are at the age of 35 or greater, as they have an increased risk of developing aneuploidy.
The sequence of the maternal serum screen is as follows.
There is first a first trimester screen which occurs at 10 to 14 weeks, and this will ultimately look for B-hCG, PAPP-A, as well as a Nuchal Translucency (NT).
We then follow this up with a second trimester Quadscreen.
This is typically performed between 15 and 21 weeks gestation, and consistent with the name Quadscreen, this is going to look for four different things, namely, the AFP, the B-hCG, the Estriol as well as the Inhibin level.
Quad Screen Interpretation
It is absolutely essential at the medical student level to be able to interpret these Quad screen values, as examiners will often ask you to point to the most likely diagnosis based on the Quadscreen.
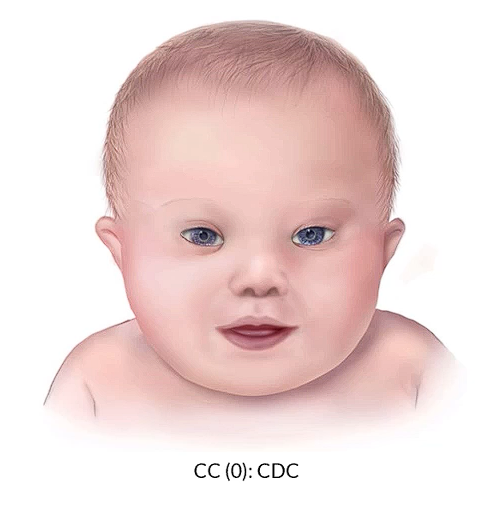
We have an example of an infant with down syndrome with the characteristic facial features in the image below.
The values for such a patient on the quad screen will include a decreased AFP, an increased B-hCG, decreased Estriol, an increased Inhibin levels.
In contrast and Edward syndrome or trisomy 18, we will see decreased AFP, a decreased B-hCG, decreased Estriol and decreased Inhibin.
Lastly, in Patau syndrome or Trisomy 13, we will see increased AFP levels, generally normal B-hCG levels, as well as normal Estriol and Inhibin levels.

©2019 BoardsMD
Therefore consistent with this, the Inhibin level can be especially helpful in differentiating these three trisomies as it is characteristically different in these different disease states, as it has characteristic levels for these different conditions, and is classically elevated in the case of Trisomy 21 or down syndrome.
AFP
Above, we mentioned that patients with Patau syndrome can have an elevated level of alpha fetoprotein, or AFP, and there are several high yield causes of an elevated AFP that we may see on a maternal serum screen.
These include inaccurate dates, which is actually the number one cause of an elevated alpha feeder protein, multiple gestation, neural tube defects, ventral wall defects, and liver tumors.
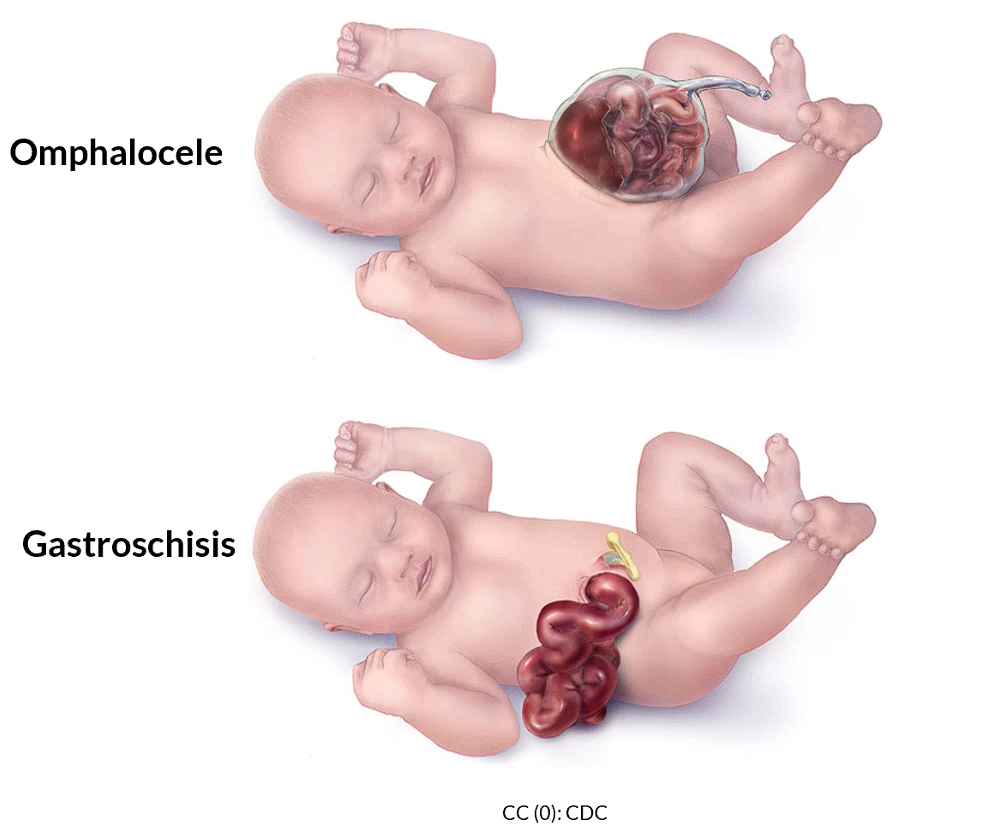
Below we have two very high yield causes of an elevated AFP, in which there is a defect in the anterior abdominal wall, namely the omphalocele in which you have this shiny sack covering the protruding abdominal contents, as well as gastroschisis which lacks this shiny covering.
Screening for Aneuploidy
As we stated previously, the purpose of this maternal serum screening is ultimately to screen for aneuploidy.
If we are to have an abnormal Quadscreen, then we can proceed with various modalities from there to further evaluate for the potential for anomalies in the fetus.
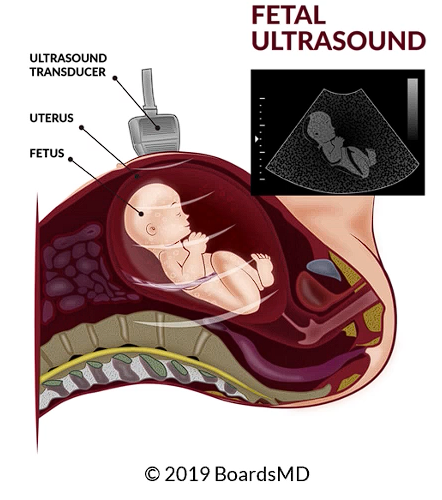
One very commonly used modality and something that is often fair game on examinations is the use of ultrasound, which we can use to evaluate the anatomy of the fetus, as well as to confirm the dates as we will review later in this article.
On examinations however, you may have to choose between the various other modalities, which include non invasive and invasive screening for aneuploidy.
If the patient desires non invasive screening for aneuploidy following an abnormal Quadscreen, then we can offer cell-free fetal DNA testing.
This cell free fetal DNA testing has very high sensitivity, but low specificity, and therefore sometimes more invasive testing may be required in the form of an amniocentesis or chorionic villus sampling.
Regardless of how we decide to proceed, however, it is absolutely essential that we make sure we respect our patient's wishes, as well as their autonomy when it comes to these important decisions in terms of screening for aneuploidy.
Cell-Free Fetal DNA
The the ideal timing for this is when there is at least a gestational age of 10 weeks. The real key indication for using cell-free fetal DNA testing is when the patient desires non invasive screening.
As we stated earlier, in this article, patients who have an age of at least 35 have an increased risk of fetal aneuploidy. Additionally, patients who have a history of aneuploidy as well as those who have had an abnormal ultrasound or abnormal Quad screen can have a follow up non invasive cell free fetal DNA as additional testing.
This may also be performed in those who desire to determine the sex of the fetus, as well as to determine Rh status.
Drawbacks
The key drawback of cell-free fetal DNA testing is that while it has a very high sensitivity, it does suffer from a low specificity, and therefore, unfortunately, it is not diagnostic.
This is in contrast to some of our other modalities, such as Amniocentesis and Chorionic Villus Sampling, in which we are more invasive, but we actually get a true sample of fetal contents in order to make an actual diagnosis of aneuploidy.
Ultrasound
Fetal ultrasound is typically done at 18 to 20 weeks in order to screen for aneuploidy. The fetal ultrasound can be extremely useful for a variety of indications, including:
- Fetal anatomy
- Diagnose pregnancy
- Investigate vaginal bleeding and early pregnancy
- Evaluate for intrauterine growth restriction, IUGR.
- Placenta Localization
- Evaluate gestational age, especially for patients who have an uncertain last menstrual period LMP
- Biophysical profile BPP, which we discuss in more detail in our article on fetal surveillance.
Biophysical (BPP)
The BPP consists of five components, including a non stress test (NST), as well as four assessments which involve the use of ultrasound in order to assess the well being of the fetus. These components are:
- NST
- Fetal Breathing
- Fetal Movement
- Fetal Tone
- Amniotic Fluid Volume (AFI)
Drawbacks
When assessing gestational age, there is a decrease in accuracy, as we have an increase in gestational age. This correlates to roughly one week of uncertainty in terms of the gestational age for every trimester that the fetus has undergone.
Examples:
- If we are in the first trimester, then the gestational age as given by ultrasound should be plus or minus one week,
- When we are in the second trimester, the gestational age as given by ultrasound should be within two weeks.
- And in the third trimester, the gestational age as given by ultrasound evaluation should be within three weeks of the actual gestational age of the fetus.
As we move deeper and deeper into the trimesters and further into the pregnancy, unfortunately, the uncertainty of our ultrasound will decrease. The best assessment of gestational age is really to do an ultrasound early in the pregnancy so that we had the least possible amount of uncertainty.
Chorionic Villus Sampling (CVS)
Moving on to the more invasive tests that we have available, we will first discuss Chorionic Villi Sampling. This is performed in the first trimester around 10 to 13 weeks.
The timing of this is very different, because it actually occurs at a different time in pregnancy than our other invasive test, which is the Amniocentesis. We have a schematic below where we could see what's going on in a case of Chorionic Villus Sampling.
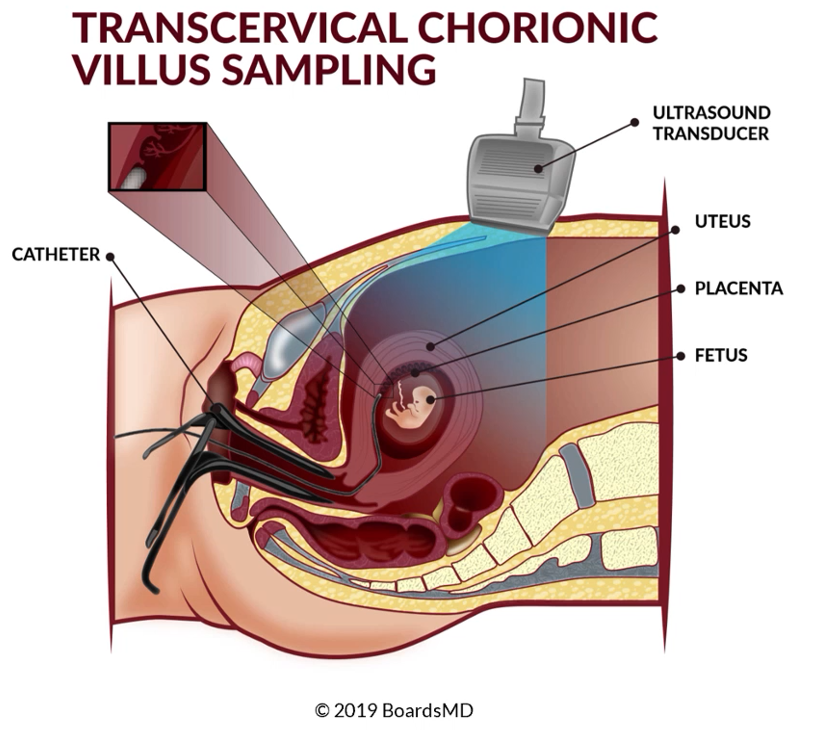
You can see that there is a catheter being fed through the opening in the speculum, where we are able to actually take a legitimate sample from the chorionic villa. You can see from this schematic, just how invasive this testing actually is, for us to be taking a sample from the chorionic Villa when we have the fetus nearby.
For this reason, Chorionic Villi Sampling is performed when we are really looking to make a diagnosis in terms of fetal aneuploidy. The risks of this procedure are otherwise too significant to justify its potential complications.
Therefore, CVS may be performed when there is an abnormal cell-free fetal DNA, as may be in the case of a patient who first desires non invasive testing subsequently has a positive cell free fetal DNA, and then proceeds to CVS.
In addition, if we discuss with our patients who have an abnormal Quadscreen, or an abnormal fetal ultrasound, and they are looking to have a diagnosis right then in there, that we can proceed to a CVS, as long as we are within this window of 10 to 13 weeks.
This timing is absolutely essential, as in the case of Amniocentesis, which will be performed at 15 to 20 weeks, we really need to keep in mind where we are at in the pregnancy in terms of choosing the appropriate diagnostic test.
Drawbacks
There are some key drawbacks of CVS that we need to be aware of.
- These include fetal loss which can occur 0.5% of the time
- Rupture of membranes, as one might expect when we are getting this close to the fetus and doing something invasive of this nature
- Preterm Labor
- Pain and bleeding
Therefore these drawbacks are really something that we need to make our patients aware of when it comes to considering CVS in this context.
Amniocentesis
In contrast to Chorionic Villus Sampling, which takes place during the first trimester at 10 to 13 weeks, Amniocentesis takes place at 15 to 20 weeks, and therefore this is going to be during the second trimester. This is going to be invasive testing.
Rather than feeding a catheter, in order to take a sample of the chorionic villus, we use a syringe to extract some amniotic fluid from the amniotic cavity. Therefore we are able to take a sample in that manner.
Because this is an invasive test, we should reserve Amniocentesis for when we really desire a diagnosis. This can be done in the case of an abnormal cell-free fetal DNA test, or can be done to follow up after an abnormal ultrasound or abnormal Quadscreen in a patient who really desires to have a definitive diagnosis.
The timing is key in terms of this diagnostic testing, as an order for Amniocentesis to be the right choice in terms of diagnostic testing for fetal aneuploidy, we need to desire a definitive diagnosis and also be in this key timing window of 15 to 20 weeks gestation. Otherwise, it is simply not going to be the answer when it comes to examinations.
Drawbacks
With the case Amniocentesis, we do have some key drawbacks, including;
- Potential for fetal loss
- Rupture of membranes
- Preterm labor
- Bowel and bladder perforation
Anti-D Immune Globulin
Indications of Anti-D Immune Globulin administration include:
- Routine prenatal care at 28 to 32 weeks
- Delivery of an RH-(+) positive baby
- Ectopic pregnancy
- Abdominal and pelvic trauma
- Second and third trimester bleeding,
- Amniocentesis/ Chorionic Villus Sampling
- External cephalic version and abortion
When we are doing an Amniocentesis/Chorionic Villus Sampling, as part of this diagnostic testing for fetal aneuploidy, there is the potential of mixing of maternal and fetal contents and the potential for ISO immunization, and therefore Anti-D Immune Globulin may be indicated in these instances.
Summary: Genetic Screening Methods
We have covered quite a bit of ground when it comes to the genetic screening methods that you may see both clinically and on examinations.
These include
- screenings for specific genetic diseases,
- the use of the maternal serum screen, especially the Quadscreen, which includes the alpha fetoprotein, B-hCG, Estriol and Inhibin levels.
When we are looking for non invasive screening tests for the purposes of fetal aneuploidy, and it is at least 10 weeks gestation, that we can use cell-free fetal DNA testing.
Ultrasound has several indications including assessment of fetal anatomy, as well as in its use in the biophysical profile (BPP). More on that and our fetal surveillance articles.
We have our invasive tests, including Chorionic Villus Sampling, which is done in the first trimester at 10 to 13 weeks, as well as Amniocentesis, which is performed in the second trimester at 15 to 20 weeks.
Stay connected with news and updates!
Join our mailing list to receive the latest news and updates from our team.
Don't worry, your information will not be shared.

