Postpartum Fever

In This Module:
- Approach to Postpartum Fever
- Atelectasis
- Endometritis
- Breast Engorgement
- Septic Pelvic Thrombophlebitis
- Mastitis
Postpartum fever is defined as a temperature greater than 100.4 degrees Fahrenheit or greater than 38 degrees Celsius which occurs at least 24 hours after delivery.
When encountering these questions on examinations, the key is to use the number of days postpartum to narrow down your differential diagnosis.
Once we know the postpartum day on which the fever is occurring, there will only be one or two options to choose from. This can be extremely useful on exam questions.
One caveat to also keep in mind is that chills and rigors immediately after delivery of the placenta are completely NORMAL in the context of pregnancy and delivery. This is something that examiners like to include to throw you off when they're writing questions.
So keep in mind that chills and rigors immediately after delivery of the placenta are normal and do not constitute any sort of post-partum fever or a disease process.
Approach to Postpartum Fever
As we approach postpartum fever, it is essential that we organize these conditions based on the postpartum day on which they occur.

©2019 BoardsMD
Day 0
Starting at the left-hand side of the Image above we have delivery. In day zero meaning in the first 24 hours, the cause of postpartum fever is going to be atelectasis until proven otherwise.
Days 1-2
Next on postpartum days 1 - 2, UTI is the most common cause of post-partum fever.
Days 2-3
On days 2 – 3 postpartum, we will see endometritis as a cause of postpartum fever.
Days 3-5
On postpartum days 3 - 5 we may see breast enlargement as a cause of postpartum fever. However, it should be noted that breast engorgement does not always cause fever.
Days 4-5
On postpartum days, 4 – 5 one of the most common causes of postpartum fever is wound infection.
Days 5-6
On days 5 - 6, the most common cause of postpartum fever will be septic pelvic thrombophlebitis
Day 7+
On day 7 and beyond the most common cause of postpartum fever will be mastitis as well as abscesses involving the breast.
There's a mnemonic to attempt to keep all these different causes of postpartum fever straight which is, wind water, womb, wean (referring to weaning involving breastfeeding), wound, and walk.
You do not necessarily need to use this mnemonic but it can be helpful in terms of keeping the different causes of postpartum fever straight and keeping the order correct.
©2019 BoardsMD
Atelectasis
This is going to present with a temperature greater than 100.4 degrees Celsius which as we said is the cutoff. For a post-partum fever.
This is going to occur on post-partum day 0, meaning in the first 24 hours following delivery
Pathophysiology
Pathophysiology in the case of Atelectasis is collapse of the alveoli, which results in cytokine release and ultimately fever
Below we have a schematic showing normal alveoli, which are plumped and filled with air abs alveoli in atelectasis where the alveoli collapse resulting in the release of cytokines, which cause fever.

Although this is more common in patients who have lung disease such as COPD, it can occur in any patient during the post-surgical period especially if they're getting general anesthesia.
Therefore, atelectasis is something important to keep in mind as we consider our differential of postpartum fever, but of course it's going to be important for post-surgical fever in general.
Diagnosis
The diagnosis of Atelectasis is typically going to be clinical.
On physical exam you shouldn’t be able to hear too much on osculation of the lungs although in some patients you may be able to appreciate rouse on physical exam.
If a chest x-ray were to be performed, we wouldn't be able to see a distinct infiltrate in the context of Atelectasis.
Management
The hallmark of management of Atelectasis is going to be incentive spirometry.
We call this incentive spirometry because as you can see in the schematic below, the patient is able to have an incentive in order to guide their breathing.
They're able to see the piston on the device which rises with each deep breath that they take.
Therefore, incentive spirometry is a great way to incentivize the patient and to motivate them as they breathe progressively deeper and ultimately prevent the progression of that Atelectasis by keeping those alveoli nice and expanded with air rather than becoming collapsed.

Endometritis
Endometritis presents on postpartum day 2 or 3 with a triad of foul-smelling vaginal discharge, a tender uterus, and fever.
In patient vignettes, there are several high yield risk factors that will predispose our patients to the development of endometritis. These include:
- Cesarean Section
- Prolonged Rupture of Membranes (PROM), which is defined as a rupture of membranes exceeding 18 hours
- Complicated vaginal delivery
- Group B Strep colonization

© 2019 BoardsMD
Chorioamnionitis
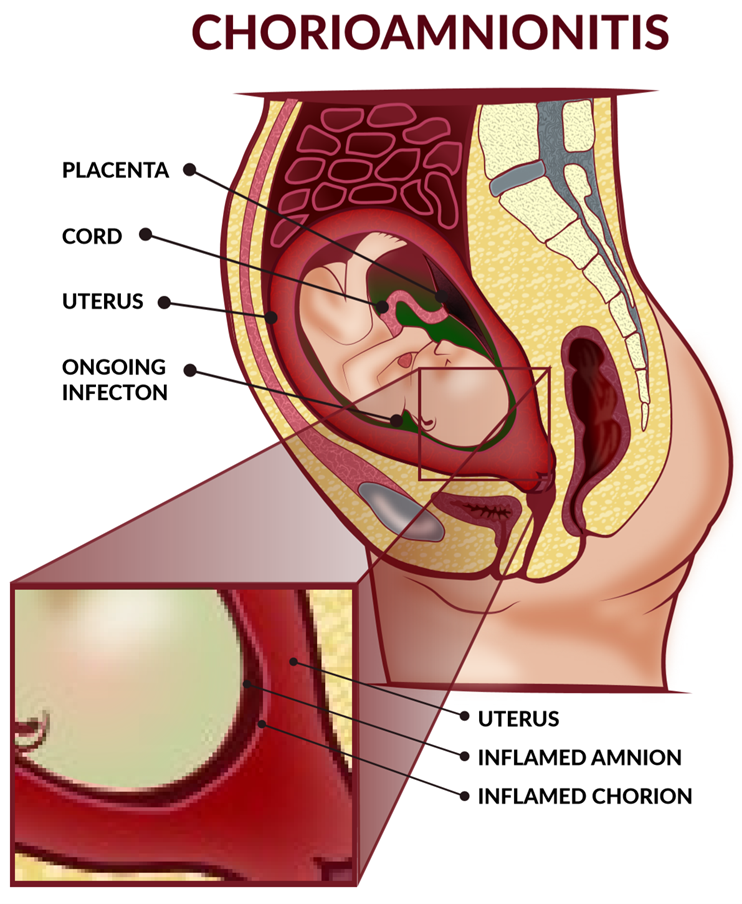
© 2019 BoardsMD
Pathophysiology
The pathophysiology of endometritis is ascending vaginal flora.
This is common in terms of all of the above risk factors, which ultimately predispose our patients to the development of this condition.
Diagnosis
The diagnosis of endometritis is going to be clinical.
If we see that triad of foul-smelling vaginal discharge, fever, and uterine tenderness especially in the context of one of the risk factors mentioned above, then we should have a high level of suspicion for endometritis.
Management
The management is going to be with IV antibiotic therapy.
Acceptable regimens include clindamycin + gentamycin or ampicillin + gentamycin in order to have broad-spectrum coverage.
Breast Engorgement
Breast Engorgement presents with bilateral breast tenderness, warmth, and erythema on postpartum days, 3, 4, or 5.
These patients may present with a low-grade fever or they may present with no fever.

Pathophysiology
The pathophysiology of breast engorgement is inadequate breast milk drainage. We have a schematic below.
You can see the clear difference here between a normal breast in which these milk glands are not engorged and an engorged breast in which these milk glands are not adequately draining their milk.
This can result in tenderness, erythema, and even postpartum fever on days, 3, 4, and 5 in a breastfeeding mother.
Diagnosis
In the case of breast engorgement is going to be clinical.
Management
We can manage these patients with the use of NSAIDS and Cold Compresses in order to help alleviate some of their symptoms.
Septic Pelvic Thrombophlebitis
This is an extremely high yield condition.
Occurs with postpartum day fever on postpartum day 5 or day 6.
It is especially important to recognize that this condition does not respond to antibiotics.
Additionally, these patients will typically have a normal physical exam with no localizing signs or symptoms.
This highlights by recognizing that postpartum days 5 and 6 are where this condition typically occurs. It's extremely high yield to keep this in mind.
Pathophysiology
Pathophysiology of septic pelvic thrombophlebitis is that during delivery there is trauma to the endothelium. This ultimately sets off the coagulation cascade resulting in the formation of a thrombus.
Bacteria then subsequently invade this thrombus resulting in septic thrombophlebitis.
Septic - referring to the bacterial portion that is invading the thrombus and thrombophlebitis - referring to the thrombus that is causing inflammation of the vein.
Below we have a schematic of a septic pelvic thrombophlebitis, where you can clearly see that there is a thrombus as well as inflammation of the vein on this patient's right ovarian vein as well as their common iliac vein.

Diagnosis
This is going to be a diagnosis of exclusion when we have a patient who presents with postpartum fever on day 5 or 6 following delivery.
We can get a CT scan of the abdomen and pelvis in order to rule out any other potential etiologies such as the formation of an abscess or anything else that may be concerning.
Management
The management of this condition is also unique in that we treat these patients with both heparin + broad-spectrum antibiotics.
The heparin being for the thrombus portion of the condition and the broad-spectrum antibiotics being for the bacterial invasion of the thrombus.
We need both of these treatments in order to adequately treat patients with this condition.
Mastisis
Mastisis will present in a patient with unilateral breast tenderness and erythema.
They may also have a mass if this is a case of a breast abscess.
This is going to present on postpartum day 7 or even deeper into the postpartum period.
Pathophysiology
The pathophysiology in the case of mastitis is breastfeeding microtrauma to the nipple, which creates openings in the areola allowing for the invasion of bacteria and ultimately mastitis and postpartum fever.
Below we have a schematic of mastitis in which we can clearly see this inflammation and erythema and redness involving the breast, however there is no discrete mass.

In the case of a breast abscess, we should have what examiners will refer to as a fluctuant mass.
That word fluctuant is extremely high yield and characteristic of absences when it comes to examinations.
The point to drive home here is that mastitis and breast abscesses will both occur on postpartum day 7 or greater.
Diagnosis
Diagnosis in the case of mastitis is going to be clinical.
There should be no fluctuance or mass on exam.
However, if there is the presence of a fluctuant mass, this is highly characteristic for a breast abscess.
Over both of these conditions, mastitis and breast abscess will occur on postpartum day 7 or even later.
Management
Management in the case of mastitis is with the use of Dicloxacillin and to continue breastfeeding. This is very high yield as the infection has no risk of being transmitted from the mother to the child. This is sufficient for the management of mastitis.
However, if there is a fluctuant mass implying that there is a breast abscess, then we can proceed with a breast ultrasound and ultimately with incision and drainage of the abscess.
Also, especially for the purposes of examinations, if there is no improvement in 72 hours with antibiotic therapy, then you should consider inflammatory carcinoma, which can also present with erythema of the breast
Just to drive home some key differences between two of our conditions causing postpartum fever;
In the case of the engorged breast, this is going to occur around postpartum day 3, 4, or 5 in and will be bilateral.
However, in the case of mastitis, this is going to occur on postpartum day 7 or greater. This is going to be unilateral as opposed to bilateral.
It is absolutely essential that we keep in mind the postpartum day on which the fever for each of these conditions occurs.
If you'd like to keep the order straight within the mnemonic, we can use the mnemonic; wind, water, womb, wean, wound, walk in order to keep these conditions straight in your mind.
Stay connected with news and updates!
Join our mailing list to receive the latest news and updates from our team.
Don't worry, your information will not be shared.

